Adverse Childhood Experiences
Understanding Adverse Childhood Experiences (ACEs)
Adverse Childhood Experiences, or ACEs, refer to traumatic or highly stressful events that occur before the age of 18—such as abuse, neglect, or household dysfunction. Research shows that ACEs are common, with nearly two-thirds of adults reporting at least one, and over one in five reporting three or more.
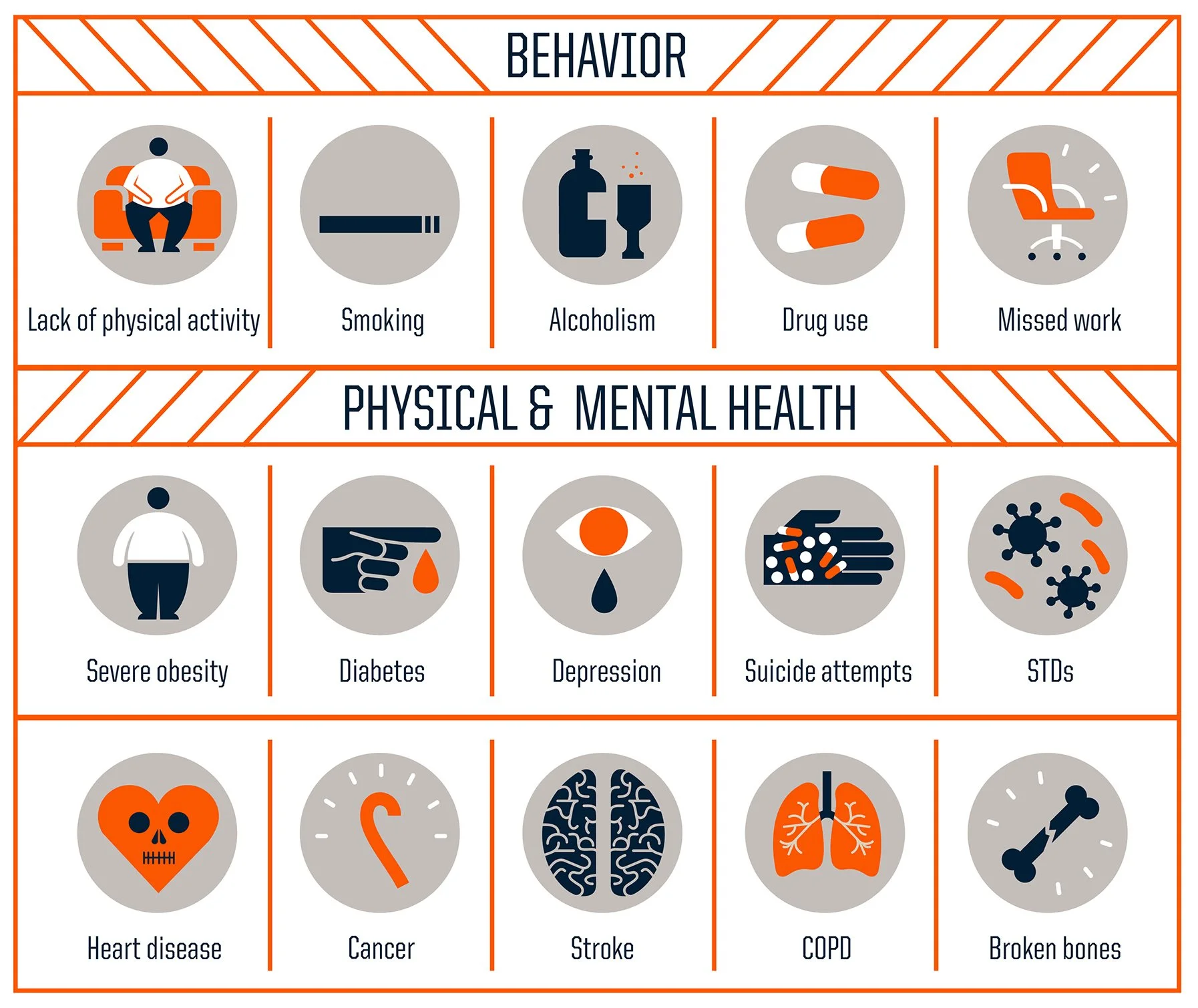
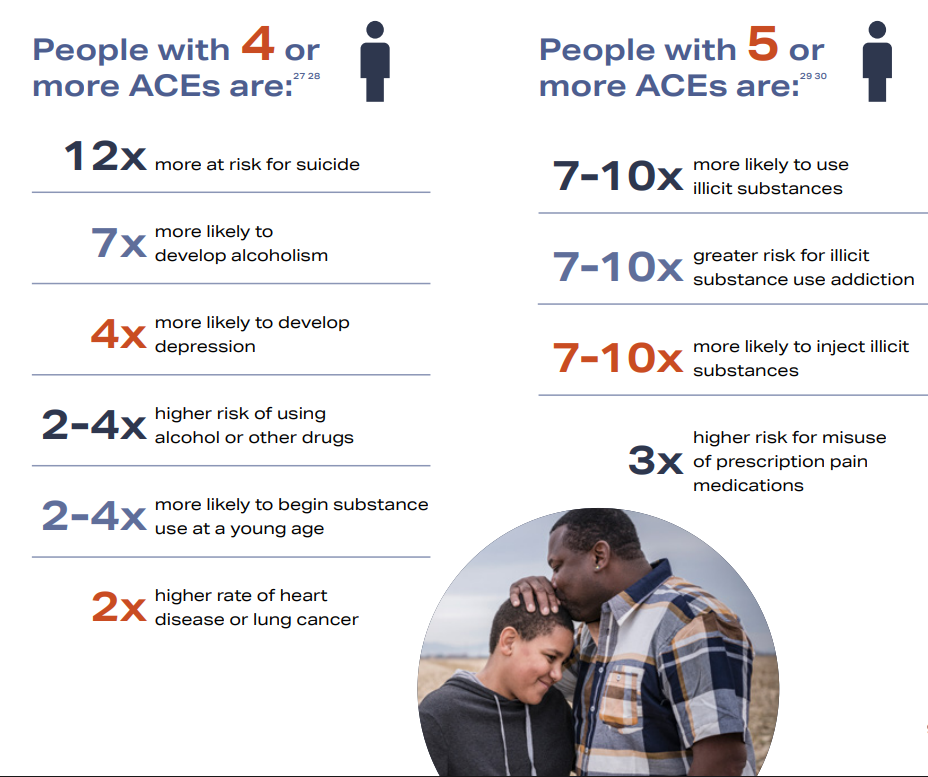
The impact of ACEs extends well beyond childhood. They increase the risk for substance use, depression, anxiety, and other behavioral health challenges, and are linked to chronic diseases later in life. The more ACEs a person experiences, the higher their likelihood of developing harmful coping strategies, including alcohol and drug use.
Recognizing the role of ACEs can be a turning point. By understanding how early experiences influence behavior, individuals can make healthier choices, seek supportive resources, and build resilience. Integrating this awareness into personal behavior change means not just treating symptoms, but addressing the root causes—fostering healing, growth, and long-term well-being.
Links to Additional Resources
Adverse Childhood Experiences and the Role of Substance Misuse Prevention (SAMHSA)
Healing from ACES: Healthy Ways to Manage Stress (English)
Healing from ACES: Maneras saludables de controlar el estrés (Espanol)
What the ACE Score Does and Doesn’t Mean (NPR)
What are ACEs Infographic (American Psychiatric Association)
About Adverse Childhood Experiences (CDC)
ACEs Risk & Protective Factors (CDC)
Positive Childhood Experiences (American Psychiatric Association)
Understanding ACEs: What are Adverse Childhood Experiences?
We Can Prevent ACEs
ACEs and Addiction: Breaking the Cycle
Adverse Childhood Experiences (ACEs) and addiction often go hand in hand. Studies show that 64% of people have at least one ACE, which significantly increases the risk of early substance use. An ACE score of four nearly doubles the risk of heart disease and lung cancer, and raises the likelihood of alcoholism by 700%. With five or more ACEs, individuals are up to ten times more likely to use illegal drugs and develop addiction.
ACEs produce consistent results regardless of type. A parent’s substance use, for example, fuels toxic stress, household dysfunction, and intergenerational trauma. Parents coping with their own childhood trauma through drugs or alcohol often pass that trauma to their children. Unless trauma is addressed alongside addiction, the cycle continues.
We know that traumatic stress leads to higher rates of depression, which in turn increases the likelihood of addiction. Stress doesn’t just affect the mind—it strains the body, raising heart rate, blood pressure, and glucose while activating “fight or flight” mode. In children, prolonged toxic stress during critical years of brain development reshapes the neocortex (decision-making and memory) and the limbic system (emotions like fear and anxiety), creating lasting vulnerabilities.
Addictive substances exploit the brain’s stress and reward systems. Drugs like methamphetamine flood the brain with dopamine, blurring the line between real and perceived threats and reinforcing survival-driven cravings. What we think of as “bad behaviors” are actually maladaptive behaviors that a person has developed to survive when supportive or trusting relationships are non-existent.
That’s why addiction must be seen as illness, not moral failure. Substances can hijack the brain so powerfully that they feel as essential as food or water. Understanding the link between trauma and addiction shifts the medical approach from “What’s wrong with you?” to “What happened to you?” Trauma-informed care emphasizes screening, empathy, and treatment of both ACEs and substance use together.
Breaking the cycle also means adults acknowledging their own trauma, seeking help, and modeling resilience for the next generation. Health care providers must care for themselves as well as their patients to truly support healing.
Addiction is a personal struggle, but recovery is possible with resilience, compassion, and community support. By understanding how stress and trauma shape behavior, reducing stigma, and offering appropriate treatment and resources, we can replace judgment and isolation with empathy and healing.
Adverse Childhood Experiences 101